Net Zero NHS
The impact of climate change represents a huge public health challenge and one that the health sector can make a significant contribution to tackling.
This is reflected in the recent commitment of all four UK health services have to achieve net zero carbon emissions. Net Zero means that the output of carbon emissions produced by the NHS is neutralised by the amount the NHS will remove from the environment.
Both NHS Scotland and NHS England have pledged to become Net Zero on their carbon emissions by 2040, with NHS England setting a target of an 80% reduction in place between 2028-2032 and Scotland setting out their plans for the next four years in their Climate Emergency & Sustainability Strategy. NHS Wales has detailed 46 initiatives in the NHS Wales Decarbonisation Strategic Delivery Plan to contribute to a net zero public sector.
The NHS is responsible for 50% of public sector emissions, which is a shocking amount. However, the NHS is able to reduce this but they need our help.
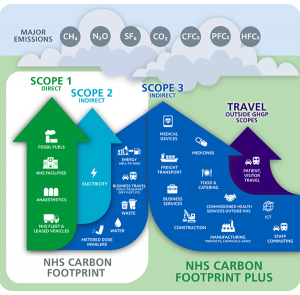
There are two parts to the CO2 production, indirect and direct.
- Direct causes are those we have direct responsibility for eg: reducing single-use plastic use and recycling within our departments and homes.
- Indirect are causes that we are not directly responsible for but are there because of the NHS requirements. eg: emissions from vehicles delivering supplies, supply chain emissions during factory production and packaging of deliveries.
UK health services aim to reduce these direct and indirect emissions by working closely with staff in their hospitals and working with supply chains that are using sustainable production methods.
More information about delivering a Net Zero health service:
- Centre for Sustainable Healthcare – Resources for Wales and England
- NHS Confederation – Sustainability in the NHS – what’s the theory and what’s the practice?
What can we do?
Orthoptists are part of a much larger AHP care group, made up of 14 distinct professions, working across the NHS. Amending the way we work and our actions at home, even in small ways, will help build towards the target of being Net Zero.
Why not try;
- Addressing the use of single-use plastics within your department? When are they necessary and where/how could this be reduced?
- Are the products we use recyclable, if not are there alternatives out there?
- Are the suppliers we’re ordering from using sustainable production and packaging methods? What is their carbon footprint?
- Is recyclable packaging being used when we post out supplies?
- Ensuring staff are using reusable mugs, bottles and cutlery.
- Reducing food packaging waste, could you buy fresh meals from the canteen instead of shop-bought packaged meals? Or bring meals from home?
- Consider how you travel to work? Could you walk/cycle, car share or use public transport?
- Ensuring electrical equipment and lighting is switched off when not in use?
- Where able, could telephone/virtual clinics be held to reduce patients need to travel into the hospital?
- Change your department lighting to LED bulbs.
- Asking patients to return aids to reuse when no longer needed. eg: planos, typoscopes or magnifiers.
- Can you apply this at home too?
These are small things that we can try and change within our own Orthoptic/Ophthalmology departments, but will overall help change the bigger picture for our NHS.
Hospitals across Britain are already beginning to make changes to the way they work. For example in Milton Keynes they have installed solar panels upon their new roof, already making savings of £18,000 off their electricity bill and reducing their CO2 emissions by 181tCO2e.
In Imperial College Healthcare NHS Trust A&E departments they have reduced the amount of single wastes plastics, especially in unnecessary cannulations. Usually, the majority of people attending A&E would be cannulated- just in case- but they found that 40% of cannulations were not needed. By reducing the number of cannulations, and introducing a process to prove cannulation is required they have managed to reduce their use by approximately 40 cannulations a day, with an estimated annual saving of £95,000 and removing 19,000 kgCO2e of waste.
You can read more examples of current case studies from NHS England here.
As AHPs are the third-largest clinical workforce in the NHS. We have the power to implement changes. If you have an idea, go with it! Talk to your line manager, your colleagues and set the ball rolling. It may influence other departments around your Hospital to do the same and even across other trusts.
Let us all work together towards achieving a Net Zero NHS.
Do you have any successes in sustainability? Please share your success and ask questions in the discussion section or send us an e-mail at: [email protected]
Further Resources
The NHS England Greener AHP Hub is now being used to support and provide information to help AHPs consider their impact and implement changes across their practice. Please follow the link to find out more.
https://www.england.nhs.uk/ahp/greener-ahp-hub/
The NHS Health Education England, e-learning for Healthcare, run a course “The Environmentally Sustainable Healthcare (ESH) Programme” to raise awareness of the Net Zero pledge and its importance. It looks into providing information for healthcare workers to be able to deliver care with financial, social and environmental sustainability. Please follow the link below to register/log in and complete the free course.
https://www.e-lfh.org.uk/programmes/environmentally-sustainable-healthcare/