The advanced clinical practice (ACP) workforce agenda is developing and moving fast. It has many exciting possibilities for our profession and we need to stay up to speed, so as not to be left behind.
Members can find links to further information and resources below [login required].
What is advanced clinical practice?
Advanced practice, while initially driven within nursing and then physiotherapy, has now been on the agenda for over a decade. Recently, there has been increasing enthusiasm for AHPs to upskill as ACPs.
ACPs are increasingly found in many areas of healthcare and are experienced, registered healthcare professionals, educated to master’s level, whose skills and knowledge allow them to “expand their scope of practice to better meet the needs of the people they care for” (HEE, 2017).
ACPs are expected to:
- demonstrate a high degree of autonomy and make complex decisions
- use their expertise and decision-making skills to inform clinical reasoning approaches
- initiate, evaluate and modify a range of interventions
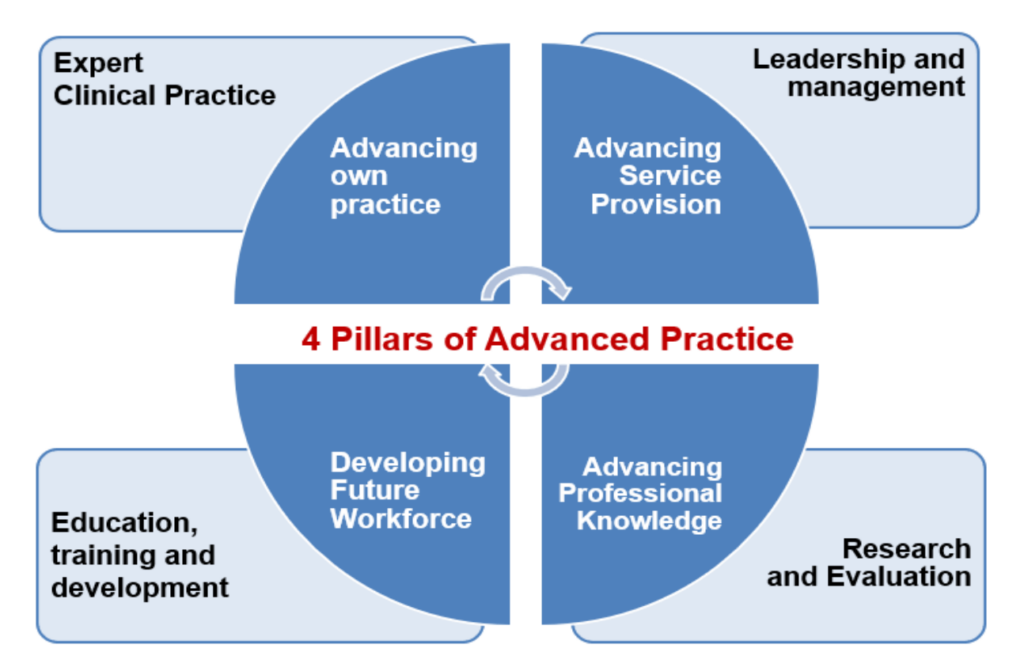
ACPs must possess the skills and knowledge across four pillars of advanced practice as set out by HEE, 2017 and these are: clinical practice, leadership, education and research. Often the clinical pillar is predominant i.e. the greater proportion of your time is spent in clinical practice. However, ACPs are expected to provide advanced skills in the other pillars too, for example, work across traditional profession-specific boundaries, implement new services and transform care pathways and take a lead in educating others, contributing to leadership as appropriate at all stages of the ACP journey.
Read more: What is advanced clinical practice?
Why is Advanced Practice Important?
There is an acute shortage of Ophthalmologists in the UK and the gap between patients’ need for appointments and Ophthalmologist clinic capacity is widening for a number of reasons, including the ageing population, the diabetes epidemic and the challenges of medical training in Ophthalmology.
By taking skilled eye-care practitioners, already working at a high level, such as specialist or advanced Orthoptists, and upskilling them in areas of practice where they can independently diagnose and treat a variety of Ophthalmology patients, we can help to meet the challenge.
Is this the same as extended roles?
No, advanced clinical practice is more than an extended role. You might have an extended role in a clinic you do once a week in addition to Orthoptics, such as in low vision or a clinical session spent on the stroke ward. But, if you were to become an ACP, you would likely spend significant time in Ophthalmology practice and, whilst you retain your base profession and HCPC registration, you might spend the majority of your working week, outside of Orthoptics, perhaps in primary, acute, or paediatric care. If you were to become an ACP, but then work most of your week in Orthoptics, you would likely be a very expensive Orthoptist to your Trust and would not be relieving the clinical burden on Ophthalmology clinics, as the ACP workforce is intended to.
Interested in finding out more?
There’s much more detail, including the routes to becoming an ACP in our resources section below.
You can also sign up for our member forum [login required].
Elizabeth’s story does not depict a typical ACP pattern of work. ACPs, unless part-time in the role, would usually be expected to predominantly carry out ACP work once qualified